The opportunity for health begins where we live, learn, work and play.
North Carolina’s Healthy Opportunities Pilot program is an unprecedented opportunity to test the integration of evidence-based, non-medical interventions into the state’s Medicaid program. The Pilots will provide non-medical services to qualifying Medicaid members across four domains: housing, food, transportation and interpersonal violence/toxic stress. Critically, frontline care managers working in Pilot regions will play an essential role in identifying members that may benefit from Pilot services, recommending appropriate services and coordinating their care. Other staff working to support Pilot operations may find these trainings helpful to support their day-to-day work.
Keep this page open while you complete the steps below.
Step 1: Create an Account
· Create a MyAHEC account.
· Already have an account? Continue to Step 2.
Step 2: Register for Courses
· Select the registration link for the course listed in the table below.
· Enter MyAHEC username and password and follow the prompts to complete registration.
· Register for each course individually by selecting the corresponding link.
Step 3: Access Course Materials
· Sign into MyAHEC.
· Select My Courses and Events.
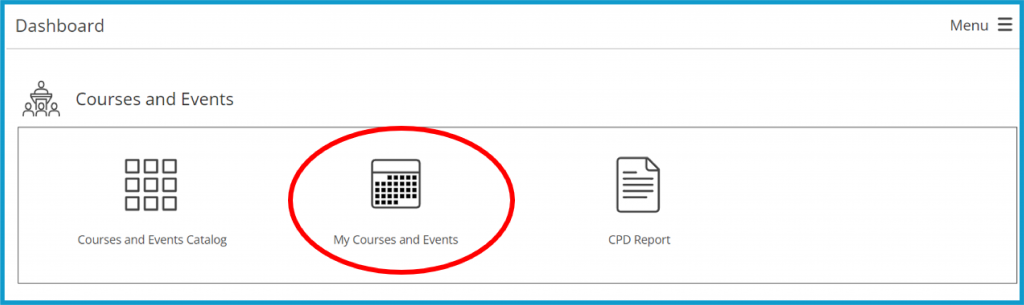
· Select Access Course and Materials.
· Select Open to launch a course.
Required and Recommended Trainings
Trainings will be continually added to this page as they are published.
REQUIRED TRAINING FOR CARE MANAGERS
| TAILORED CARE MANAGERS | |||
| Release Date/Last Updated | Title | Select the link to register for your course or to view slides & recordings. | Course is required for Care Mangers |
| October 20, 2023 | Healthy Opportunities Pilot Training for PIHPs and Tailored Care Managers Part 1 | Register | This course is intended for Care Managers who will provide Tailored Care Management to Healthy Opportunities Pilot members. |
| November 20, 2023 | Healthy Opportunities Pilot Training for PIHPs and Tailored Care Managers Part 2 | Register | This course is intended for Care Managers who will provide Tailored Care Management to Healthy Opportunities Pilot members. |
| STANDARD PLAN CARE MANAGERS | |||
| Release Date/Last Updated | Title | Select the link to register for your course or to view slides & recordings. | Course is required for Care Mangers |
| November 17, 2022 UPDATED October 2023 | How Care Managers Can Choose Appropriate Interpersonal Violence Services | Register | YES |
| March 21, 2023 | Healthy Opportunities Pilot: How Care Managers Can Choose Appropriate Interpersonal Violence Services Part 2 | Register | YES |
| March 17, 2023 | How Care Managers Can Obtain Pilot Consent | Register | As Care Managers transition to using the consent form released in Spring 2023, this course is required. |
| N/A | NC AHEC Diversity, Equity, and Inclusion (DEI) for Primary Care Clinical Providers and Non-clinical Staff | Module 2 – Cultural Humility | MAHEC | YES |
RECOMMENDED TRAINING FOR CARE MANAGERS
| Release Date/Last Updated | Title | Select the link to register for your course or to view slides & recordings. | Course is required for Care Mangers |
| October 23, 2024 | Duplicative Medicaid and Healthy Opportunities Pilot Services | Register | |
| August 7, 2024 10 a.m. LIVE WEBINAR | Supporting Survivors of Interpersonal Violence: Practice Session for HOP Care Managers | Register | |
| June 26, 2024 | Healthy Opportunities Pilot: Screening for Adverse Childhood Experiences for Care Managers | Register | |
| June 14, 2024 | Healthy Opportunities Pilot Housing Rights 101: Tenant and Landlord Responsibilities | Register | |
| May 9, 2024 12:00-1:00pm | Duplicative Medicaid and Healthy Opportunities Pilot Services – Live Webinar | Register | |
| October 31, 2023 | Intimate Partner Violence – Creating A Culture of Care for Survivors | Register | Note: HOP Care Managers can register for FREE, contact whitney.gordon@mahec.net for code. |
| October 31, 2023 | Intimate Partner Violence – Best Practices in Intimate Partner Response | Register | Note: HOP Care Managers can register for FREE, contact whitney.gordon@mahec.net for code |
| January 20, 2023 | How Care Managers Can Choose Appropriate Health Related Legal Supports | Register | |
| December 27, 2022 | How Care Managers Can Choose Appropriate Toxic Stress Services | Register | |
| December 8, 2022 | Understanding the Medical Respite Cross Domain Service | Register | |
| September 20, 2022 | How Care Managers Can Choose Appropriate Housing Services | Register | |
| September 2, 2022 | How Care Managers Can Choose Appropriate Food Services within the Healthy Opportunities Pilot Programs | Register | |
| September 2, 2022 UPDATED September 2023 | How Care Managers Can Choose Appropriate Transportation Services, Version 2 | Register | |
| August 22, 2022 UPDATED September 2023 | Tracking Enrollee Progress, Reviewing Service Mix, and Reassessing Pilot Eligibility | Register | |
| March 9, 2022 | Assessing Member Eligibility for Participation in the Healthy Opportunities Pilots | Recording and Slides | |
| February 25, 2022 | Deeper Dive on Pilot Responsibilities of Frontline Care Managers | Recording and Slides | |
| February 11, 2022 | The Role of CIN Care Management Teams in the Healthy Opportunities Pilots | Recording and Slides | |
| N/A | Using Motivational Interviewing to Support the Healthy Opportunities Pilots | SEAHEC | |
Training for Human Service Organizations (HSOs)
| Release Date/Last Updated | Title | Select the link to register for your course today | Required for HSOs |
| June 30, 2024 | Healthy Opportunities Pilot Overview for Human Service Organizations | Register | |
| March 17, 2023 | Sensitive Services for HSOs and Pilot Staff; Privacy & Confidentiality for Survivors | Register | YES |
Other HOP-related Trainings
| Release Date/Last Updated | Title | Course materials | Recommended For |
| May 3, 2023 | CHW Specialty Training Program: Introduction to Healthy Opportunities Pilots for CHWs | Register | Community Health Workers |
| May 16, 2022 | Evidence Base Roundtable Series #6, Intimate Partner Violence | Slides | |
| May 12, 2022 | Evidence Base Roundtable Series #5, Network Lead Pilot Region Overview | Slides | |
| April 29, 2022 | Evidence Base Roundtable Series #4 Housing, Transportation and Legal Support | Slides | |
| April 21, 2022 | Evidence Base Roundtable Series #3, Food and Pilots Evaluation | Slides | |
| April 12, 2022 | Evidence Base Roundtable Series #2, SIREN | Slides | |
| April 6, 2022 | Evidence Base Roundtable Series #1, Kickoff | Slides | |
February 15, 2023 | Healthy Opportunities No Wrong Door Approach to Enrollment | Recording and Slides | Primary Care Providers and Advanced Medical Homes |
| December 16, 2022 | Healthy Opportunities Pilots: Local Health Department Care Manager Pilot Engagement | Slides | Local Health Departments |
Building the skills and capacity for diversity, equity and inclusion (DEI) takes time to learn and integrate into patient care. For this reason, it is recommended that Healthy Opportunities Pilot staff complete additional trainings, such as Implicit Bias, Structural Racism, Communication in Healthcare, and Microaggressions.